
Breaking Down Barriers: Oklahoma Women
- Rachel Armstrong, Metriarch Support Staff
- April 15, 2021
- Access to Quality Care
More women are in the workforce than ever, yet still, women remain chiefly responsible for duties at home. Women rise up in the face of societal pressures to run a household, work demanding jobs, and deal with constant emotional labor through it all, more commonly known as the “mental load.” Many are dealing with concerns over their health, and yet are unable to receive necessary care. 24% of all adult women in Oklahoma report poor or fair health status.1 Let’s take a look at some of the barriers to accessing comprehensive care, and how we are breaking them down.
Oklahoma Women Reporting Poor or Fair Health Status, 2016-2018.
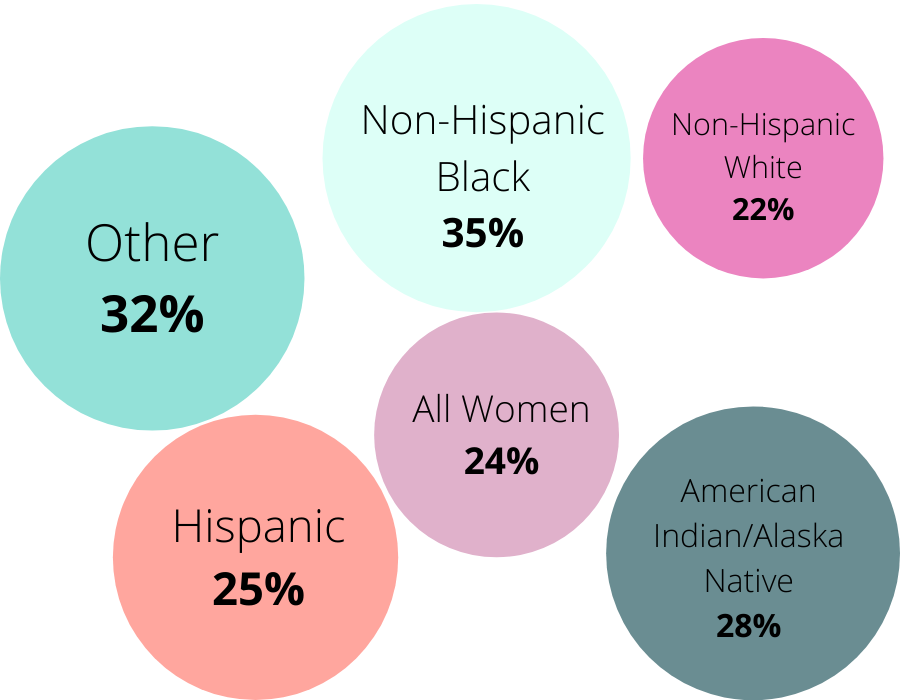
Source: Kaiser Family Foundation. Note: Not Significant Data for Asian and Native Hawaiian or Pacific Islander
Notably, Americans are more concerned with paying for any serious illness they may face rather than the illness itself. This is completely understandable since the American health care system is notorious for sending patients into debt due to medical costs.2 Oklahoma is no exception, with 30% of the state reporting unpaid medical debt in 2017. Although legislation like the Patient Protection and Affordable Care Act (aka PPACA aka ACA) has recently tried to make healthcare more attainable and inexpensive,3 there is still a long way to go. Oklahoma women face many barriers to accessing high-quality, comprehensive care. Filling in the gaps in our health system is critical to ensuring everyone receives the care they need.
19 percent of women in oklahoma are uninsured.
The second highest rate in the nation.
One of the most glaring barriers to care is the high number of uninsured women in Oklahoma. This percentage has stayed relatively stagnant over the last 6 years. Most people receive health insurance through their employer, but many people, including those who work part-time, or for small businesses, are often unable to get coverage.
On June 30th, 2020, Oklahomans voted to pass State Question 802 (SQ802). This amendment to the State’s constitution will expand Medicaid, also known as SoonerCare in Oklahoma, to provide healthcare to those who previously fell into the aptly named coverage gap. The coverage gap referred to the population with income between the current Medicaid eligibility level and the Federal Poverty Level, roughly between $5,104 and $12,760 for individuals. In Oklahoma, this means there are nearly 200,000 people who can now gain access to health care coverage!
Most are childless adults, who have been historically excluded from Medicaid eligibility. No one is more deserving of access to healthcare than another. Prioritizing access only when a woman becomes pregnant represents the pervasive belief that women’s health is restricted to motherhood. Policies like SQ802 will help all Oklahomans lead healthier, happier lives.
Questions still remain as to how exactly Medicaid expansion will happen. One proposed idea is to utilize a privatized managed care model, meaning healthcare services would be organized and delivered only through certain providers. However, this idea is hotly contested due to the potential harm managed care could cause to the interests of patients and providers alike. These conversations about accessing healthcare clearly aren’t over just because SQ802 passed.
Consistent care must be provided to everyone throughout the lifespan.
Expanding health insurance eligibility is one step towards increasing access to healthcare, but it is not the only step that must be taken:
- Providers must be held accountable. Medical mistrust is deep-rooted within many communities—and for good reason. There is a long history of systemic discrimination in medicine that has led to significant health disparities in marginilzed communites. Currently, as many as 39% of Hispanic women in Oklahoma report having no personal doctor, as opposed to 16% of Non-Hispanic white women. Disparities in healthcare such as this will only become more severe if ignored. Systemic discrimination in medicine must be actively combatted by our heatlhcare providers.
- Increasing diversity in healthcare will help build trust and sustained relationships with people who are historically underserved. The racial and ethnic diversity of the country is not reflected in medical professionals. As it stands, nearly 20% of the U.S. population is Hispanic and/or Latinx, but less than 6% of doctors are. When the clinician workforce does not represent the population it serves, communities can more easily become marginalized and cut off from valuable services.
- Providers must become culturally competent in building balanced relationships with patients. Building a relationship with a doctor is daunting. Telling anyone the details and symptoms of our bodies requires a high level of trust, and expressing these feelings to someone you just met can be intimidating. A primary care doctor is trained in facilitating these tough conversations, but nothing can substitute the bond that grows over time, and with respect.
Women are often providers of consistent emotional support to those around them, but this may come at a cost to their own well-being. Access to comprehensive preventative care can empower women to practice healthy behaviors both for their physical and mental health.

